
Prevalence
Arterial Ulcers (AUs) are among the most common type of ulceration, accounting for 25% of lower leg ulcers.1,2 AUs occur commonly on foot, around the ankle or lower leg. AUs can be distinguished from venous leg ulcers (VLUs) by color and appearance. VLUs appear red, shallow and irregular in shape, while AUs boundaries are round and well defined, and the surrounding skin is cold to the touch.3,4
Risk Factors
The primary risk factors for AUs include age, hypertension, dyslipidemia, obesity, sedentary lifestyle, diabetes and family history.5 African Americans are at higher risk than Hispanics and non-Hispanic Whites.6

Pathophysiology
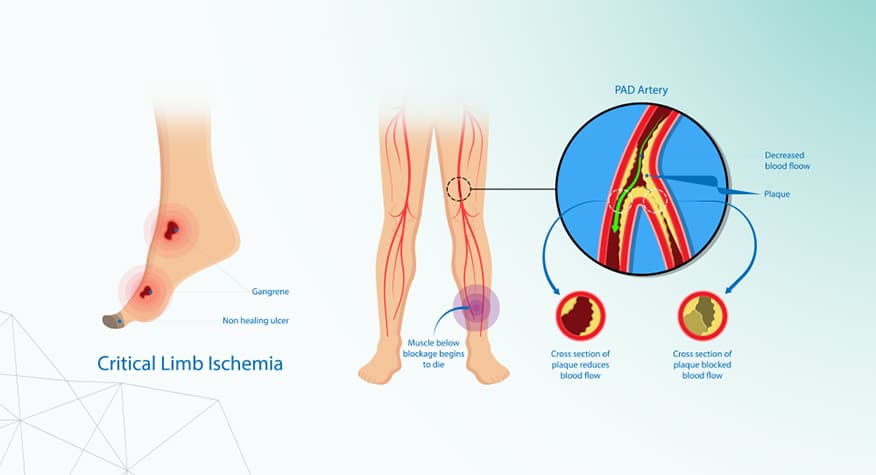
AUs are caused by arterial insufficiency or poor perfusion to the skin and soft tissues.7 Arterial insufficiency is caused by high blood pressure and narrowing of the arteries due to atherosclerosis, deposits of circulating lipids to the vessel walls.

Assessment
The clinical diagnosis of AUs is based on the evaluation of clinical history, diminished or absent pulse, nocturnal claudication and changes in skin color. The diagnostic studies include transcutaneous oxygen measurement (TCOM), toe brachial index (TBI), arteriography, and arterial dropper studies.

Prevention and Treatment
Patient education along with early management of blood pressure, cholesterol, triglyceride and blood glucose levels can help minimize the risk for developing arterial ulcers. The primary treatment for AUs is arterial revascularization by endovascular treatment or open arterial reconstruction to increase blood supply to the affected area.
References
- Adeyi A, Muzerengi S, Gupta I. Leg ulcers in older people: A review of management. BJMP. 2009; 2(3):21-28.
- Nagaratnam N, Nagaratnam K, Cheuk G. Chronic leg and foot ulcers in the elderly. Geriatric Diseases. 2017:1-6.
- Janowska A, Dini V, Oranges T, Iannone M, Loggini B, Romanelli M. Atypical Ulcers: Diagnosis and Management. Clin Interv Aging. 2019;14:2137-2143. Published 2019 Dec 10. doi:10.2147/CIA.S231896.
- Grey JE, Harding KG, Enoch S. Venous and arterial leg ulcers. BMJ. 2006;332(7537):347-350. doi:10.1136/bmj.332.7537.347.
- Hess, Cathy Thomas BSN, RN, CWOCN Arterial Ulcer Checklist, Advances in Skin & Wound Care: September 2010 – Volume 23 – Issue 9 – p 432 doi: 10.1097/01.ASW.0000383218.26406.4b.
- Ghidei W and Collins TC. African Americans and peripheral arterial disease: a review article. ISRN Vascular Medicine. 2012.
- Spentzouris G, Labropoulos N. The evaluation of lower-extremity ulcers. Semin Intervent Radiol. 2009;26(4):286-295. doi:10.1055/s-0029-1242204.
- Tautenhahn J, Lobmann R, Koenig B, Halloul Z, Lippert H, Buerger T. The influence of polymorbidity, revascularization, and wound therapy on the healing of arterial ulceration. Vasc Health Risk Manag. 2008;4(3):683-689. doi:10.2147/vhrm.s2186.
