Utilization of Advanced Imaging Modalities and Artificial Intelligence in Mitigating Clinical and Financial Risks Associated with Treatment and Management of Pressure Injuries
By Raphael Yaakov and Anthony Pinto
Keywords: pressure injuries, hospital-acquired conditions, quality gap, cost-benefit, internal rate of return, value analysis, artificial intelligence, digital imaging solution, advanced wound imaging
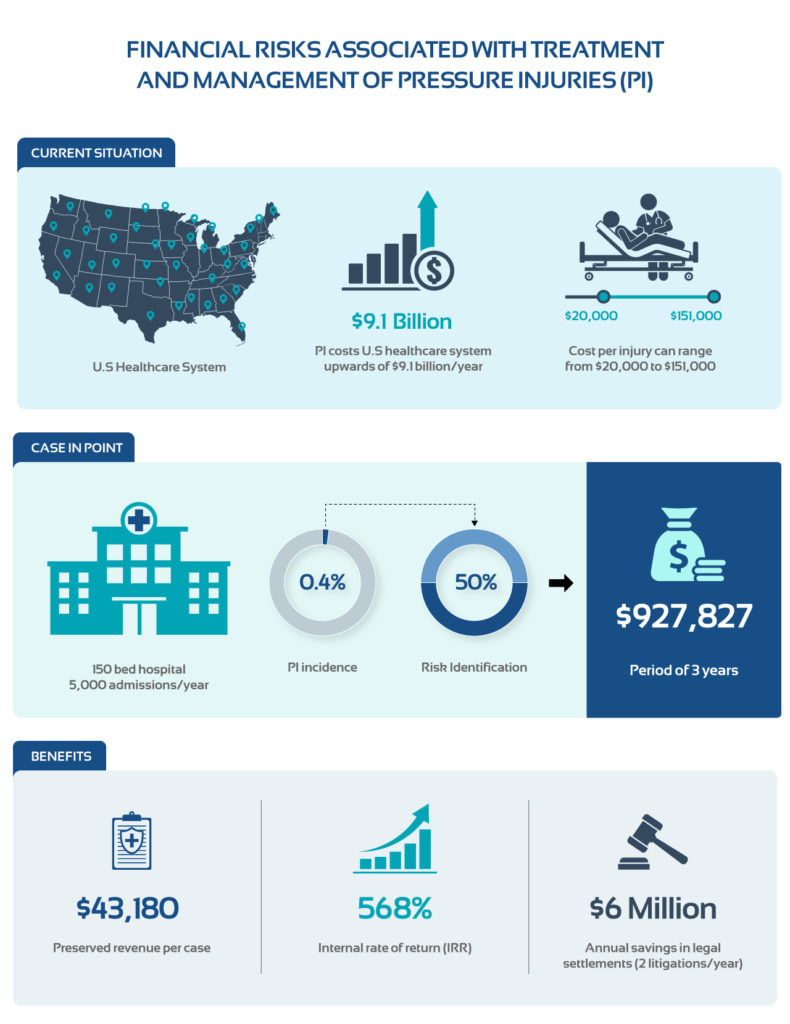
Pressure injuries (PIs) remain one of the most challenging issues, costing the U.S healthcare system upwards of $9.1 billion per year.1 The cost per injury can range from $20,000 to $151,000, often leaving hospitals with the full financial burden.2 Over the past few years, the Centers for Medicare and Medicaid Services (CMS) began reducing reimbursement for hospital-acquired conditions (HAC). The penalties for HAC are based on the hospital’s performance on key quality measures, which includes patient safety, rates of PIs, healthcare-associated infections (HAI), and adverse events. CMS publicly reports HAC data on the Provider Data Catalog website. This can have far-reaching consequences beyond reduced payments; it can impact ratings and irrevocably damage the reputation of a hospital.
Furthermore, there are imminent legal implications associated with PIs. Lawsuits are on the rise in both acute and long-term care settings, accounting for 25% of all litigation cases in skilled nursing and assisted living facilities.3 PI litigation cases are expensive with settlements ranging from $1 million to $5 million per case.4,5 It is not surprising to find that lawsuits for PIs are common and second only to wrongful death.6 Medical malpractice litigation adds billions of dollars in annual costs to hospitals and has contributed to the rising cost of healthcare. Thus, the importance of appropriate assessment and management of PIs cannot be overemphasized.
The quality gap typically emerges due to lack of documentation on patient admissions. Lack of access to standardized tools adds to the problem. To close the quality gap, it is essential to have a clinically validated solution for assessment and documentation of PIs. Institutional practices, however, are not standardized and vary across practices. Providers continue to rely on conventional methods which are cumbersome and prone to error. In fact, manual measurements of PIs can overestimate surface area for complex and irregularly shaped ulcers.7 While acetate tracing offers greater reliability over the ruler method, the process is time-consuming and not always feasible for a high-volume clinic that frequently encounters large complex PIs.
Objective methods that provide accurate and timely assessment of PIs are essential for early implementation of optimal prevention and treatment measures. Despite advancements in digital imaging modalities and proliferation of mobile technology, adoption and utilization has been limited in clinical practice. Implementation of a digital imaging solution can streamline clinical workflow and improve efficiency. Beyond practical advantages, such as non-contact measurement, improved documentation, audit trails and reduction in clinic and patient cycle time, digital wound management offers a robust method to assess complex ulcers and monitor changes with ease and flexibility.
Furthermore, digital imaging solutions can help reduce millions of dollars in medical and legal costs. Based on Medicare’s estimate of the cost of PIs, this would potentially represent about $43,180 per case in preserved revenue.2 Consider a 150-bed hospital with the PI incidence of 0.4% among 5,000 admissions per year.‡ Assuming a risk identification of 50%, the initial capital investment can help preserve nearly $927,827 over a period of 3 years.* This provides a cost/benefit ratio of 9 and internal rate of return (IRR) of 568%, indicating a superior rate of return. Additionally, proper assessment and documentation would help avoid an excess of $6 million annually in legal settlements even if hospitals only reduced 2 litigations per year.** The value of digital health solutions extends beyond the bottom line. It enables providers to work more productively, manage and treat PIs efficiently, while improving institution’s quality metrics.
There is growing opportunity to leverage data and artificial intelligence (AI) to inform and guide clinical decisions. AI modeling, for instance, can help predict the risk for PIs among critical care patients, assist in PI staging, as well as assess which patients could benefit from early intervention. AI can also help with resource planning. For example, hospital administrators can determine how many specialty beds would be required. AI models are able to produce detection accuracy of up to 95% in experimental settings.8,9 Digital imaging solutions, AI and advanced analytics are essential tools in the required armamentarium for the prevention and management of PIs. Timely and appropriate utilization of advanced imaging modalities can not only help lower financial and clinical risks but also enable evidence-based clinical decision-marking and improve the overall quality of care.
‡ The device costs are estimated based on the median capital investment and recurring annual costs for digital imaging solution. Note that some imaging modalities may require additional use fees. The admission rate per year is estimated based on American Hospital Association Statistics Report (2019).
*The present value (PV) of the expected benefit (EB) over a given time period (t) is given by the formula: PV= (EB/ (1+% Discount Rate)t ). Net PV= ∑PV Future Benefit – ∑PV Future Costs. Expected benefit was computed using Medicare’s estimated cost of PIs to approximate revenue preserved, however, the actual costs may vary based on staging or early detection.
**Assumes 3 million in legal settlements per year. Calculation based on the average cost of litigation per case.5,6
References
- Walker CA, Rahman A, Gipson-Jones TL, Harris CM. Hospitalists’ Needs Assessment and Perceived Barriers in Wound Care Management: A Quality Improvement Project. J Wound Ostomy Continence Nurs. 2019;46(2):98-105. doi:10.1097/WON.0000000000000512
- Agency for Healthcare Research and Quality. Are we ready for this change? 2014. https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu1.html
- Volchok J. Avoid Wound Litigation. VOHRA Wound Physicians. How To Avoid Wound Care Litigation? 2019. https://vohrawoundcare.com/avoiding-wound-litigation/
- Davani R. Pressure Ulcer Lawsuit Settlement. 2022. https://nursinghometruth.com/bedsore/pressure-ulcer-lawsuit-settlement/
- Kreisman R. $5 Million Jury Verdict for Stage 4 Bed Score and Wrongful Death. 2019. https://www.robertkreisman.com/nursing-home-lawyer/5-million-jury-verdict-for-stage-4-bed-sore-and-wrongful-death/
- Petrone K and Mathi L. Pressure Ulcer Litigation: What is the Wound Center’s Liability. Today’s Wound Clinic 2017. https://www.hmpgloballearningnetwork.com/site/twc/articles/pressure-ulcer-litigation-what-wound-centers-liability
- Shah A, Wollac C, Shah JB. Wound Measurement Techniques; Comparing the Use of a Ruler Method, 2D imaging and 3D Scanner. J AM Coll Clin Wound Spec. 2015; 5(3):52-57.
- Bates, D.W., Levine, D., Syrowatka, A, et al. The potential of artificial intelligence to improve patient safety: a scoping review. Npj Digit. Med. 4, 5. 2021.
- Swerdlow M, Guler O, Yaakov R, Armstrong D.G., Simultaneous Segmentation and Classification of Pressure Injury Image Data Using Mask-R-CNN. AI in Medicine. Submitted 2022.
The views and opinions expressed here are those of the author and do not necessarily reflect the official policy or position of any other agency, organization, employer or company.
About the Authors
Raphael Yaakov serves as the VP of Clinical Development at eKare, Inc.. His experience spans across public health, clinical research, and technology. He has helped support key initiatives in patient education programs, global epidemiological surveillance to managing phase I-IV multinational drug and device studies. He completed his undergraduate course work in life sciences at the Pennsylvania State University and holds a MS with a concentration in pharmacoeconomics and outcomes research from University of the Sciences in Philadelphia.
Anthony Pinto is a customer success leader focused on the customer journey – from the sales process, through implementation and post-install success. Prior to joining eKare, Anthony spent 9 years with SigmaCare (now MatrixCare), creating and building their customer success organization that focused on both retention and growth in the EHR space. Anthony currently serves as VP of Business Development & Customer Success.
